Implementation of a Far North Queensland Virtual Fracture Clinic: the patient’s experience
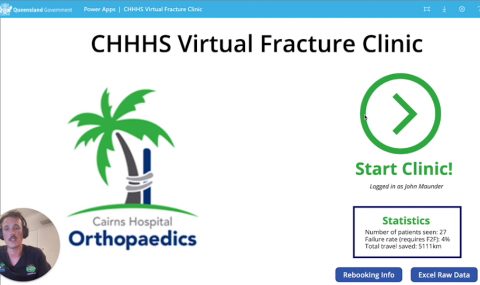
Principal Investigator: Dr John Maunder MBBS, BEng(Hons), MTrauma, GradCertSci - Orthopaedics Principal House Officer at Cairns Base Hospital; Principal Supervisor: Associate Professor Tim Dwyer MBBS, FRACS(Orth), PhD- Orthopaedic Surgeon at Cairns Base Hospital
PROJECT SUMMARY
Rationale: Virtual fracture clinics (VFCs) have been proven successful in several institutes worldwide. They challenge the typical in-person model of health care by treating selected injuries remotely (via a single phone consult). A VFC has unique advantages in remote Australia, by reducing and/or eliminating what are often significant travel distances and costs (both to the patient, and the health service via travel subsidies).
An audit of our current fracture clinic model identified that we review approximately 90 new patients per week, on average travelling 50km (1- 998km). Based on UK literature, a conservative estimate would suggest that 50% of these could be managed via a VFC model.
Currently, there are no prospective studies confirming the efficacy of a VFC. In addition, travel savings (cost or distance) have never been reported. In Australia, only a single retrospective review of VFCs exists - this was conducted at a metropolitan centre and did not include distance or patient satisfaction as outcomes.
Aims: Demonstrate the effect of a VFC in a remote setting by measuring the primary outcomes of patient satisfaction, cost savings, and reductions in travel time / distance. Secondary outcome measures will include reduction in emergency department representations and complications.
Hypothesis: A VFC will result in significant cost savings, as well as reduction in travel time and distances for patients with fractures in regional areas of Far North Queensland with high patient satisfaction.
Design: Prospective cohort study (Level II).
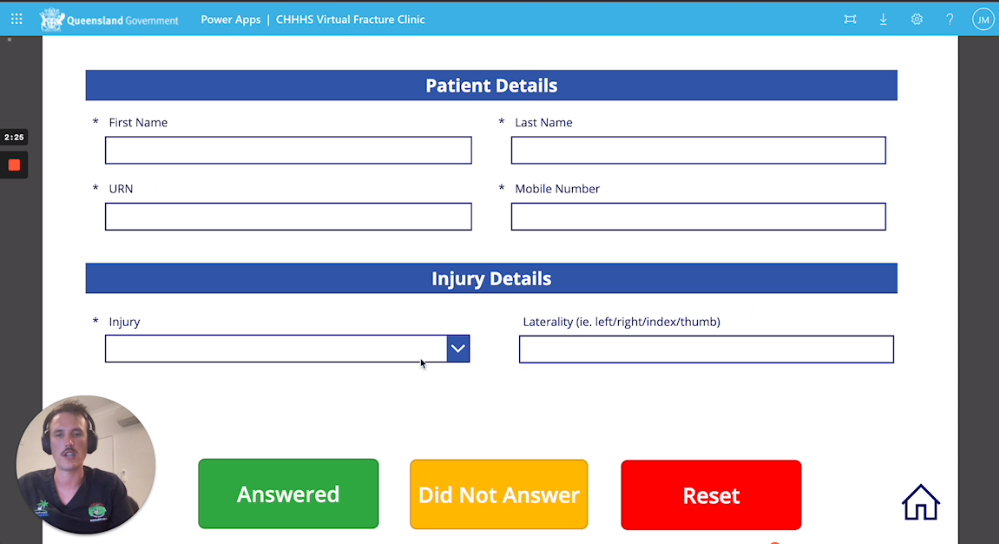
Method: Conditions which have a strong evidence base to support exclusive non-operative treatment without repeat reviews or imaging will be chosen by a working group. Patients with these conditions will be followed up via telephone by an orthopaedic registrar. At this virtual clinic, patients will either be discharged with education (phone, SMS, or email), or referred to another medical or non-medical service (including back to an in-person fracture clinic). Immediately after their consult patients will be sent a satisfaction survey in addition to contact information and education materials about their injury. Chart reviews will be conducted at three months post injury to ensure patients have not re-presented or experienced a complication.
A one-month pilot will be conducted to refine appropriate conditions, education materials, and system processes. The study will then run over 3 months, treating an estimated 500 patients.
Analytics plan: Means and standard deviations will be calculated for cost, distance travelled and satisfaction.
App created to significantly reduce time and costs